12 Jun Early orthodontic intervention in children
Advantages of 6 month braces! Cork dentist Dr Tony O’Connor explains why early orthodontic intervention is imperative in tackling a range of developmental problems among children
Dental healthcare professionals are encouraged to assess orofacial myofunctional disorders (OMDs) in their patients. Interest in myofunctional therapy by sleep experts is compelling dental healthcare professionals to revisit the evaluation of myofunctional disorders. Many dental practices pay little attention to OMD and the role they play in craniofacial growth, airway and overall general health.
Negative craniofacial growth can be attributed to OMD1. The consumption of soft processed foods has also had a negative impact on craniofacial growth2. Improper dentofacial growth and development can contribute to a restricted upper airway and associated sleep disorders. Since experts agree that 70 per cent of facial growth is complete by age seven1 3, early identification and timely treatment of OMD may decrease the risk factors for sleep disordered breathing (SDB) and, of course, the need for possible extractions for orthodontics later.
Winter is here and with it the advent of winter bugs and viruses, keeping doctors’ surgeries busy with sick children and stressed parents. A seven–year–old child presents to the local GP complaining of a sore throat and chesty cough. The child is also bed–wetting and mum wonders if the cold resulted from lying in the wet bed? The doctor examines the child and diagnoses inflamed tonsils. Another course of antibiotics is prescribed, yet again. When mum asks why the tonsillitis keeps recurring, the doctor suggests a referral to an ENT surgeon. The doctor reassures mum that, while upsetting, the child is young, and will probably grow out of wetting the bed.
Once recovered from the illness, mum brings the child to the dentist. She is concerned about some mild crowding of lower incisors. She reminds the dentist that the child tends to “gag”, and is quite a fussy eater, to the point that most foods have to be mashed or pureed. During the consultation, she expresses her concern about her child’s tooth grinding, particularly at night.
The dentist examines the child, reassuring mum that there are no cavities, and explains that bruxing is nothing unusual at that age. Mum is told that the mild incisor crowding will be monitored, and should orthodontic treatment be required, it would be best to wait until all the permanent teeth erupt at approximately 11 or 12 years of age.
This common medical/dental scenario is all too often played out. However, if viewed from an “Airway Health” perspective, there are many clues to indicate that the child’s dentofacial growth may not be proceeding normally.
These red flags include; recurrent tonsillitis, chesty cough, bed–wetting, mild crowding of lower incisors, a gag–reflex, and a soft diet. In fact, all the clinical signs and symptoms above.
How could the above medical and dental complaints negatively impact on cranio–facial growth and result in not only malocclusion, but a myriad of supposedly “unrelated” health problems for the child? If parents and healthcare professionals alike are trained to recognise the many obvious signs and symptoms of inadequate cranio–facial growth, and learn to adopt an early interceptive philosophy, could it be conceivable that many common paediatric health issues would be alleviated or ameliorated?
If this were possible, and it is, the significance should not be underestimated by parent, health professional, or government, as the overall physical and emotional wellbeing of the child would be greatly enhanced. Not only would this new protocol have an enormous positive financial impact on government health spending (Heckman report) but the number of children presenting with crooked teeth and poorly developed faces in tandem with the many airway–related health problems could be greatly reduced.
There is now a lot of scientific evidence to show the effects of mouth breathing and OMD on craniofacial growth and our overall health4. Studies on mouth breathing by Harvold 5 in the 1970s revealed the harmful effects on facial growth in monkeys. Researchers inserted latex plugs into the noses of rhesus monkeys in order to evaluate the effects of mouth breathing on facial structure. The monkeys were forced to switch from nasal breathing to mouth breathing. To compensate for the inability to breathe through the nose, the monkeys developed postural changes, which were followed by soft tissue changes.
The cranio–facial muscles then caused various malocclusions, including retrognathia, prognathisim and anterior open bites, when forced by the new functional demand. The interaction between oral and facial structural growth and muscle activity starts early in development and continues through childhood. Chronic oral breathing is an important clinical marker of orofacial muscle dysfunction, which may be associated with narrow high vaulted palates, nasal obstruction leading to negative changes in facial structure4.
These negative changes are reflected in the skeletal malocclusions, such as Class 2 or Class 3, and open or closed bites. The resulting dentitions that evolve also reflect negative growth patterns such as dental crowding, (mild or severe), crossbites, etc.
Harvold’s experiments, although crude, proved that changing the oral environment caused a structural change in the form of the face. To put it another way, when function changed, form changed. Anthropologists believe that modern man (Homo sapiens) has been around for about 250,000 years, only a very short time on the evolutionary clock. For most of this time we were hunter–gatherers and it was only in the last 12,000 years that farming and agriculture became established. This more sedentary lifestyle brought with it a change in diet.
Anthropologists have shown that changes in facial form began around this time. In fact they can prove that the human face started to “shrink” or retract about 10,000 years ago. This pace has accelerated since the Industrial Revolution. Our Paleolithic ancestors had much more forward facial profiles and examination of skulls show broad dental arches – with inter–molar widths of 55mm – and plenty of room for all 32 teeth, even with an extra 1cm behind the wisdom teeth (Daniel E Lieberman).
WHAT DOES A “SHRINKING FACE” MEAN? DOES IT MATTER?
The human head, composed of the cranium, is made up of 22 bones. Eight bones of the neurocranium (occipital, two temporal, two parietal bones, sphenoid, ethmoid and frontal bone), and 14 bones of the viscerocranium.
Space for the brain itself is almost fully established at birth, with neural growth having occurred rapidly in utero. However growth of the face (or viscerocranium) is only approximately 35 per cent established at birth. Growth of the face is quite fast over the next few years reaching almost 60 per cent by age four, and finishing by around 12 years of age.
As well as having sufficient room to accommodate all 32 teeth, our Paleolithic ancestors had remarkable dentitions with few cavities and no malocclusion. This is sadly not the story today, yet the genotype remains the same. Growth of the facial structure is very much influenced by the oral environment, correct growth is in a forward and downward direction from the cranial base6.
We need space for the internal organs, the tongue, the nasal passage, the oropharynx and space to accommodate our larynx, thyroid gland, and of course trachea and oesophagus, and let’s not forget all 32 teeth. And, most importantly, accommodate the airway space. The mature oropharyngeal airway should be between 10 and 12mm. When it is less or becomes blocked, we are going to experience a disturbance in breathing. Anything that interferes with oxygen supply to our organs is not good.
If the required architecture does not develop correctly, compromises will be reflected in form and function. I like the statement “Anatomy is the platform on which physiology is based”. If the anatomy is underdeveloped we can only expect changes in our physiology later. We are now seeing a rise in the amount of people suffering from hypertension, heart disease, diabetes, obesity, depression, sleep apnoea (OSA), sleep disordered breathing (SDB), stroke, Attention Deficit Hyperactive Disorder (ADHD) and other behavioural problems.
THE EMERGENCE OF DENTAL SLEEP MEDICINE
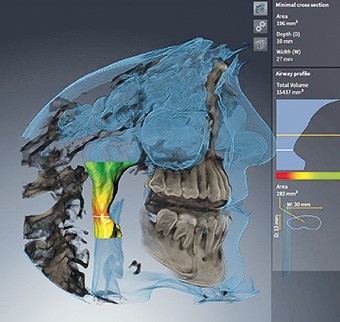
Many dental practices in the US have incorporated dental sleep medicine into their practices, because numerous patients are presenting with the aforementioned issues. There are many correlations between poor cranio–facial growth, malocclusion, and the above health issues. Upper airway imaging has allowed us to understand the biomechanical bases for OSA and mouth–breathing.
The new CBCT imaging software programs provide accurate mapping of the oropharyngeal airway space. This can be very important in designing orthodontic treatment plans. In cases of impeded airway it is important to recognise the structural imbalance and take adequate steps to achieve harmony and facial balance in conjunction with the restoration of physiologic functions. Sleep disorders have been estimated to affect 50–70 million people in the US and are linked to increased risk for hypertension, diabetes, obesity, depression, heart attack and stroke8.
Furthermore the risk of a serious car accident increases when the driver is sleepy. There are now numerous reports of serious car and rail accidents attributed to drivers falling asleep behind the wheel. Hundreds of millions of dollars are spent each year in medical costs related to sleep disorders.
WHAT IMPACT DOES SLEEP–DISORDERED BREATHING HAVE ON CHILDREN?
In children, snoring, mouth breathing, and obstructive sleep apnoea can have a negative effect on behaviour, as well as the ability to pay attention in school. In a large multi–year cohort study (11,000 patients) it was shown that in children from six months to seven years of age, snoring, OSA, and mouth breathing contribute to increased risk of ADHD, peer to peer behavioural problems, increased aggression and anxiety9.
Dr David McIntosh, an ear, nose and throat surgeon based in Australia, has an interesting website (http://www.entspecialists.com.au) in which many of the recent research papers on the airway issue and how it impacts on the brains of young children are reviewed.
The consequences of poor sleep add up over time. Studies are now showing that when sleep architecture is affected on a regular basis, Alzheimer’s disease leading to dementia increases. During the period of deep sleep, our brains are cleansed of metabolic waste that builds up during the day. Research shows that patients suffering from Alzheimer’s disease have a build–up of a protein called amyloid. This affects the communication system within the brain. In studies of mice where oxygen levels decreased, their brains started to show a build–up of amyloid10 11. There are many causes of a bad night’s sleep, one of them is sleep apnoea12.
IT’S NOT JUST THE BRAIN THAT SUFFERS
Apart from all the problems with brain function, SDB in children also has adverse effects on the heart and blood pressure15. In fact, it may very well be that high blood pressure experienced in adulthood originates from sleep problems as a child16.
The seven–year–old boy brought to visit the doctor and dentist could well have been showing signs of Sleep Disordered Breathing. Regular bouts of tonsillitis is associated with mouth breathing. Further questioning may have revealed a snoring issue too?
Teeth grinding or bruxisim is an indicator of an airway problem. Historically it was associated with a psychological problem… stress? What we know now is that 80 per cent of children who grind their teeth and who have an airway problem, stop grinding their teeth once the airway problem is fixed. Maybe they are stressed because they can’t breathe properly13.
This seven–year–old also displayed crowding of lower anteriors, another indicator of poor facial growth and a developing malocclusion. The child’s bed–wetting is also another indicator of a narrow palate.
An interesting book called Naso–Respiratory Function and Craniofacial Growth edited by James A McNamara Jr, features a chapter written by orthodontist Dr Robert M Rubins. It states: “The recognition that crisis care in medicine is the least effective and most expensive therapy has focused the attention of health providers on prevention.
“Similarly, in dentistry, the understanding of the pathology of dental caries and periodontal disease has led to a preventive orientation: control of plaque. Yet, in orthodontics it is common practice to allow the course of detrimental growth to proceed until its virtual completion before commencing treatment.
“By age four the craniofacial skeleton has reached 60 per cent of its adult size. By age 12, the age when most orthodontists initiate treatment, 90 per cent of facial growth has already occurred (Meredith 1953). To wait until 90 per cent of a deformity is established before instituting treatment is not consistent with a preventive philosophy.”
PATIENT 1
Patient presented age 10, complaining of protruding upper front teeth. She had a mouth breathing pattern, lips apart most of the time and a bilateral tongue thrust. She is undergoing orthotropics and myofunctional therapy. She will be at least another year in treatment. Due to her poor myofunctional habits i.e. mouth breathing, both upper and lower jaws are underdeveloped. Her upper front teeth are not really protrusive at all, her upper and lower jaws are in fact retruded. Orthotropics aims to correct this negative growth pattern.
PATIENT 2
Patient presented age nine. Mum complaining of his crooked teeth. Child is a chronic mouth breather and was very hyperactive prior to treatment. He has a vertical growth pattern with both upper and lower jaws retruded in the face.
The patient’s airway space was compromised and he used to be a restless sleeper. No sleep study was undertaken. He is presently undergoing orthotropics and now much improved. Treatment is ongoing.
CONCLUSIONS
It is obvious from the above information that we need to screen our young patients earlier.
Screening can start with the dental hygienist or nurse taking the medical history and asking specific questions.
Screening can begin with questions: (only a few listed here)
- Birthing process, normal, induced, how long mum was in labour, whether forceps delivery or suction used?
- Breast feeding? Bottle feeding?
- Did the baby experience colic?
- Bedwetting, sleep posture, night terrors?
- Snoring, drooling on pillow?
- Teeth grinding, gagging?
- Sleep apnoea? (Epworth sleep questionnaire)
- Mouth breathing or nasal breathing?
- Tongue–tie or lip–tie, scalloping of tongue?
- Mallampati score, indication of oropharyngeal airway
- Tongue thrusting, orofacial myofunctional disorders (OMD)?
- Facial profile
- Gummy smile
Other records such as X–rays and photos also help to tailor a treatment plan for the young patient. Awareness of the above listed signs and symptoms should help us to identify if a child’s facial growth is not proceeding normally.
To quote Dr John Flutter, a dentist practicing in Brisbane, Australia: “Nothing will change if nothing changes.”
REFERENCES
1. Proffit WR Contemporary Orthodontics 3rd St Louis: Mosby ,2000.
2. Price W (ed).Nutrition and Physical Degeneration 8th ed La Mesa, Ca: Price–Pottenger Nutrition Foundation,2008:55
3. Development of Lower Jaw:Meredith HV. Growth in head width during first 12 years of life. Paediatrics 1953 Oct:12(4) 411–29
4. Jefferson Y. Mouth breathing: Adverse effects on facial growth, health, academics and behaviour .Gen Dent 2010 Jan–Feb; 58(1): 18–23.
5. Dr Egil Peter Harvold: Harvold EP, Tomer BS, Vagervik K, Chierici G. Primate Experiments on Oral Respiration. Am. J.Ortho.1981 Apr;79(4):359–72. Miller AJ, Vagervik K, Chierici G. Sequential Neuromuscular changes in rhesus monkeys during the initial adaptation to oral respiration. Am J. Ortho.1982 Feb;81(2):99–107
6. Moss M The Primacy of functional matrices in orofacial growth. Dental Practitioner 19:63–73.
7. The American Academy of Pediatric Dentistry. Guidlines on periodicity of examination, Preventive Dental Services, Anticipatory Guidance/Counselling, and Oral treatment for infants, children and adolescents. Clinical Guidline.2013 v 35/No6:114–22.
8. Commmitee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: Unmet Public Health Problem, Washington DC: The National Academics of Sciences, 2006.
9. Bonuck K et al. Pediatrics.2012 Apr;129 (4):e857–65. Sleep–disordered breathing in a population–based cohort: behavioural outcomes at 4 and 7 years.
10. Daulatzie MA. Neurotox Res 2013 Aug;24 (2):216–43. Death by a thousand cuts in Alzheimer’s disease: Hypoxia—the prodrome.
11. Tspanou A et al. Dement Geriatr Dis extra 2015 Jul 10; 5 (2):286–95
12. Gagnon K et al. Pathol Biol (Paris) 2014 Oct; 62 (5): 253–40
13. Efterkharian A. Et al , Int J.Pediatr Otorhinolaryngol. 2008 Apr;72(4):509–11, Bruxism and adentonsillectomy. Difrancesco RC et al, Int J Pediatr Otorhinolaryngol 2004 Apr;68(4):441–5, Improvement of Bruxism after T and A surgery.
14. The Evolution of The Human Head by Daniel E. Lieberman
15.Nisbet LC et al. Sleep Med Rev. 2014 Apr;18(2): 179–89
16.Vlahandonis A et al. Sleep Med Rev. 2013 Feb; 75–85.
- Non–nutritive sucking habits.